The space has a great role in our life. Our body is composed of five basic components: the earth, water, air, fire (heat or temperature) and the sky or space. The space within and outside our body is must for the existence of life. The outer space is composed of air (mixture of gases), vapours, finer particles, microorganisms, radiation, light, cold and heat. The composition of environment influences our breathing, metabolism and physiology. Our body reacts in a variety of ways to the external space and the environment possessed by it. In fact the particles floating in the air or transmitted through it may cause allergic reactions, infections, hot or cold skin burns or even skin cancer. All activities of human beings or animals are space oriented.
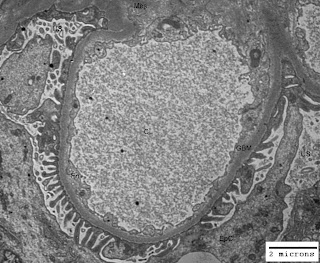
Just think of the life without space and you would understand its importance. Our body is like a tube open from both ends. You may appreciate space in your mouth (oral cavity), throat, nostrils, ears and lungs. In addition to these gross pockets of space there are hollow organs like heart (four chambers are there for blood flow regulation), gall bladder, urinary bladder and uterus (in females). Other examples of space within our body are cranial cavity, visceral cavity and cavities around all vital organs. There are micro-spaces in glandular tissues, alveoli of lungs, blood vessels and nephrons (glomeruli have capillary lumen and urinary space) in kidneys. In some of the renal disorders there are ultrastructural alterations in the areas/volumes of these micro-spaces within the kidneys leading to altered renal physiology and renal function. The figure-1 below illustrates normal urinary space (US) and capillary lumen (CL) or capillary space in a normal kidney; and figure-2 illustrates congestion of capillary lumen (CL) due to deposition of subendothelial deposits (SeD) in a kidney affected by lupus nephritis.
Figure-1: Ultramicrograph of a capillary loop from a normal human kidney illustrating normal urinary space (US) and capillary lumen (CL) with normal thickening of glomerular basement membrane (GBM); Uranyl acetate and Lead citrate stain.
Figure-2: Ultramicrograph of a capillary loop from human kidney affected by lupus nephritis, illustrating congestion of capillary lumen (CL) due to deposition of subendothelial deposits (SeD) with normal urinary space (US) but irregular thickening of glomerular basement membrane GBM); Uranyl acetate and Lead citrate stain.
In the illustration cited above you have seen the alteration in the space within the renal glomerulus. Abdominal tumors, brain tumors, polyps in the uterus, enlargement of spleen and liver, all these lead to functional as well as physiological changes in the body of a patient due to impact on space within the body.