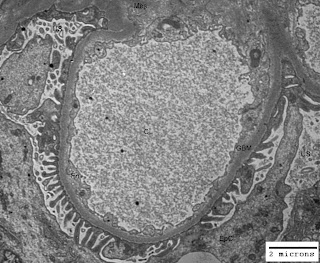
Correlation of clinical and laboratory features is must for an accurate diagnosis and type of a kidney disease (renal disease) or glomerulonephritis. An experienced nephrologist can make a diagnosis of glomerulonephritis from thorough history, physical examination, urine examination and microscopy of urinary sediment. The assessment of presenting features of the patient, such as nephritic or nephrotic syndrome is important. However, the decision on the type of glomerulonephritis can not be based on the clinical and laboratory features; as the nephrotic syndrome may occur with any histological glomerulonephritis, and nephritic syndrome is the outcome of proliferative glomerulonephritis. So the ultimate diagnostic tool is renal biopsy and its light and fluorescent microscopy as well as ultrastructural study by electron microscope.
The interpretation of clinical features in the light of histological diagnosis of renal biopsy helps the clinician to detect any systemic disease associated with the renal disease (kidney disease). Majority of the patients with suspected glomerulonephritis need renal biopsy evaluation. However, in children with nephrotic syndrome; if there is no microscopic hematuria (blood in urine) and red cells' or granular casts, renal biopsy procedure may be avoided initially. In patients, who do not respond to steroid therapy; renal biopsy investigation is must. There are around one million glomeruli (1x106 glomeruli) in each kidney and at least 5 glomeruli should be included in the renal biopsy evaluated histologically to achieve a diagnosis of glomerulonephritis.
Radiological and laboratory investigations in glomerulonephritis:
The clinical presentation, urine-analysis and microscopy findings, and presence of a normal upper & lower urinary tract on intravenous pyelography (IVP: a radiological investigation) or ultrasonography without any renal scarring could be indicative of glomerulonephritis, but there could be a need for renal biopsy.
Immune system associated investigations:
Our body is equipped with a multitasking immune system composed on lymphocytes, antibodies and complement system. The immune system always defends our body internally against a variety of infections and pathological conditions; and assessment of its components and abnormal products produced by it helps in diagnostic conclusions. Complement system of our body is composed of 9-components and boosts the body defense in association with cellular components. The blood level of complement components C3, C4 and C1q may be reduced or normal in some renal diseases. Low total serum complement, C3, C4 and C1q levels are observed in glomerulonephritis associated with circulatory immune complex disorders like systemic-lupus erythematosis (SLE), bacterial endocarditis and serum sickness. Normal levels of C4 and C1q but decreased level of C3 is generally observed in membranoproliferative glomerulonephritis (MPGN) and dense deposit disease of the kidney.
Following investigations are considered important to ascertain the diagnosis and type of glomerulonephritis:
Investigations for likely diagnosis of glomerulonephritis:
- Clinical presentation
- Urine analysis (proteinuria, hematuria and electrophoresis)
- Microscopy of urinary sediment
- Intravenous pyelography (IVP: Radiological investigation)
- Abdominal ultrasonography.
Investigations for likely type of glomerulonephritis:
- Estimation of serum complement components' level
- Detection of circulating immune complexes
- Detection of auto-antibodies such as anti-nuclear antibodies (ANA), anti-DNA antibodies and anti-glomerular basement membrane antibodies (anti-GBM antibodies)
- Renal biopsy
Investigations for assessing the implications of glomerulonephritis and monitoring the effect of therapy:
- Determination of 24 hour urinary protein
- Determination of level of serum proteins
- Determination of serum cholesterol and/or lipid profile
- Determination of serum creatinine, blood urea and serum electrolytes.